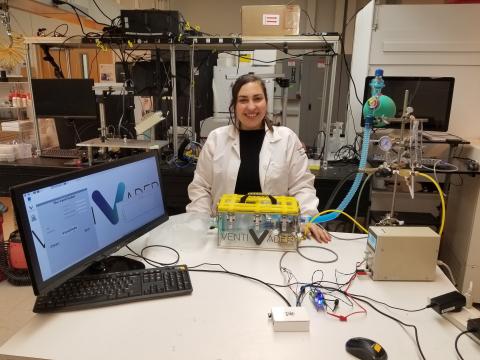
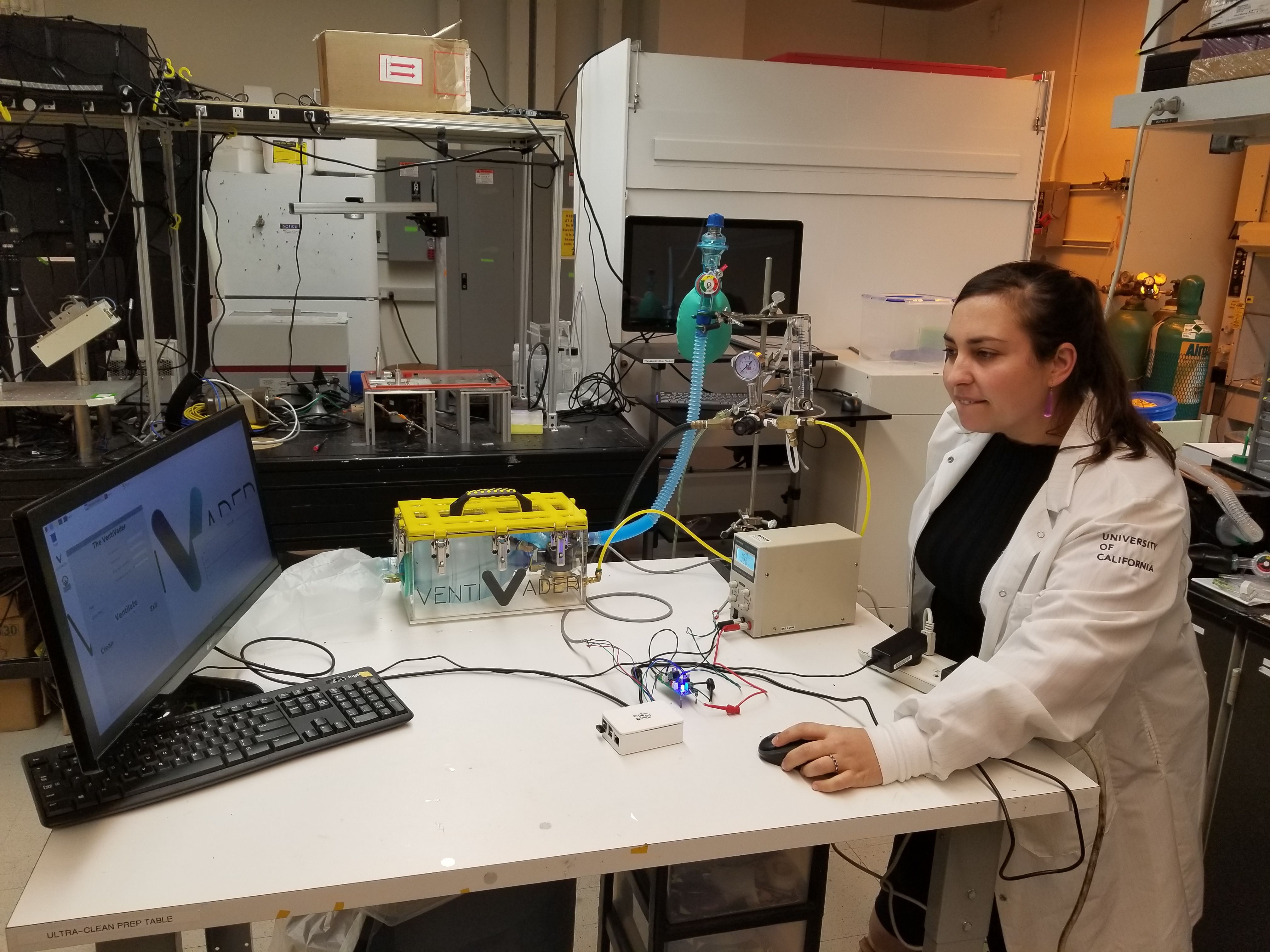
Alexandra (Sasha) Perebikovsky is an ARCS Scholar Alumna who received her PhD in Chemical and Materials Physics at University of California, Irvine in May 2020. She and two other colleagues have developed a low-cost ventilator that can be produced for $100 or less—that’s tens of thousands of dollars less than the cost of commercial ventilators on the market today. Their device, affectionately named “VentiVader,” is portable, easy to operate and uses compressed air available in every US hospital. Unlike other low-cost solutions, this ventilator can control tidal volume and pressure for safer and more effective patient outcomes. An application for emergency FDA approval is under way, as are discussions with Mexico and India—two countries with a severe, unmet need for ventilators.
Currently the VentiVader team is working on finishing the Android and iOS apps to operate the ventilator. They have also developed an analog version of the device that can be operated without any expensive digital components. The team is working on making the ventilator usable in "extreme point-of-care" environments, such as rural areas in developing countries that do not have access to primary-care facilities and common hospital infrastructure. For example, the new rural health kiosks being developed in India are one of the areas being targeted. These kiosks use low-cost and point-of-care devices to provide critical health services to rural communities without proper healthcare infrastructure.
In addition to her work with the VentiVader team, Sasha leads the Microfluidics team at Sensor-Kinesis Corporation (SKC), a point-of-care medical diagnostic company. SKC is working in collaboration with the laboratories of Dr. Philip Felgner and Dr. Marc Madou at UC Irvine to develop an automated serological test for COVID-19. “We hope we can produce this test as an automated, inexpensive, and point-of-care instrument so we can accelerate the development of personalized medicine and treatment that takes into account differences in individual response,” Sasha says.
This test will be able to detect sixty-seven antibodies for several respiratory viruses, including SARS-CoV-2. These antibodies are critical to see who in the population has been exposed to the virus, even if they are asymptomatic, and how their body has responded to that exposure.
The results of this test are critical on two levels: On the individual level and the community level. On the individual level, the test will provide information about an individual infection and the response that a person’s immune system has to that viral infection (immune system fingerprint). This is critical because not only does it tell whether someone has a disease, it also can be used to guide and personalize treatment. For example, for plasma transfusions, antibody profiles are required.
On the community level, a seroprevalence study can be done by testing many individuals in a specific community or society and obtaining a serological profile for each person. This testing gives scientists, doctors, and policymakers critical information regarding disease transmission and characteristics, including why certain groups are affected differently from others. This profile can also be used to study the effectiveness of introduced vaccines and accelerate their development.
Sasha is appreciative of the opportunities she received as an ARCS Scholar. “I have not only been able to finish my dissertation but also have had the time to help develop COVID-19 diagnostics during this critical time.”
Along with three other ARCS Foundation Scholars, Sasha participated on the ARCS Scholar COVID-19 Panel on June 12, 2020. Below are Sasha’s responses to follow-up questions on her projects to combat COVID-19.
Q: Tell us more about how and by whom VentiVader would be used in an extreme point-of-care environment. You mentioned a shortage of healthcare professionals in these areas. Doesn’t it take a highly trained professional to ventilate a patient?
A: My PhD adviser and I have had a strong collaboration with Dr. Satadal Saha, who is responsible for building up a network of "rural healthcare kiosks" in India. These kiosks are meant to bring healthcare and modern medicine to extreme point-of-care rural areas that have limited access to primary-care facilities. Together, we wanted to bring automated and simple systems that can easily be operated by trained local women, who would help administer treatments in these facilities with the assistance of doctors meeting with patients through telemedicine. The idea is that these places could act as "bridge" sites to properly ventilate patients in the time it takes to get proper primary care. The ventilator has many built-in safety functions, including pressure and flow sensors that can control tidal volume, pressure of air delivered, and breaths per minute, to safely ventilate patients while a trained medical professional advises on the settings to use over telemedicine.
Q: What are the failure modes for VentiVader?
A: The main failure modes might come from improper feedback from the pressures and flow sensors integrated into the VentiVader. It is important to be able to control the pressure and tidal volume while ventilating a patient, so these sensors failing can be a pretty big deal. The other failure mode includes the inability to have proper digital or internet connections in certain extreme point-of-care settings. As a result, we have someone working on an analog-controlled version of the VentiVader. We are also working on "ruggedizing" the VentiVader for better functions in extreme environments.
Q: What kinds of conditions would be early candidates for enhanced treatment by the antibody fingerprint results, and how would treatment be adjusted as a result of this information?
A: The antibody fingerprint results can provide a crucial repository of data on different groups and societies exposed to COVID-19. First, I envision this diagnostic to be crucial in determining public policy, such as when a community should begin reopening and what the scope of that reopening should be. Second, these results are necessary for personalized treatments such as plasma transfusions, which have been tested as treatments for COVID-19. A serological profile can give doctors a better idea of who might be candidates for these experimental treatments.